Ten years ago, if you talked about meeting your significant other online, ordering a meal through an app, or asking your car for the fastest way home, you were definitely outside the norm.
Today, however, technology is prevalent throughout our social and workplace activities. It should be that way for our healthcare activities too.
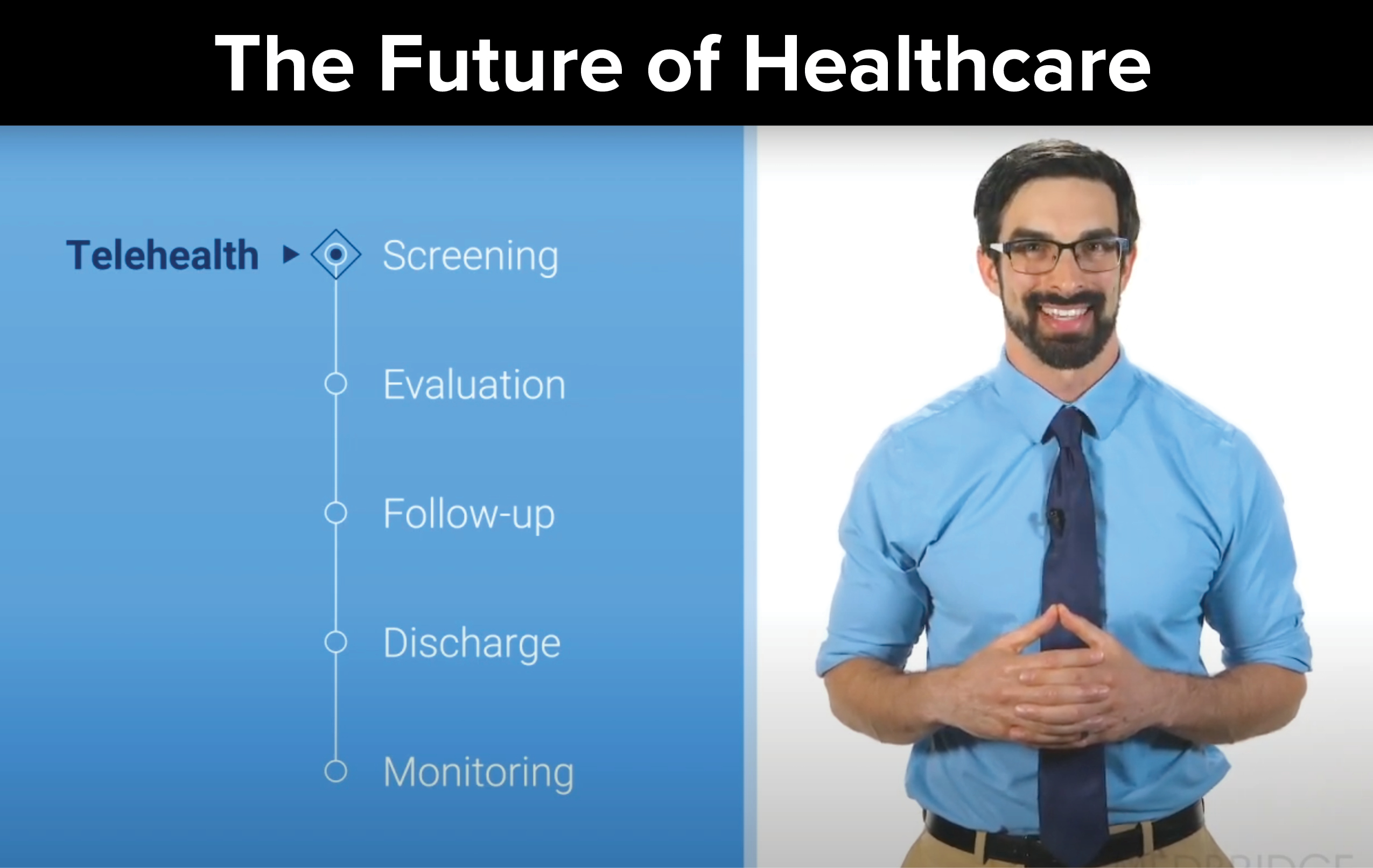
Introducing Telehealth
The healthcare landscape has seen many challenges in the past decade, including increased costs and decreased reimbursement. Now, during the COVID-19 pandemic, reduced patient volume and trickling appointments are a common occurrence. Many practices are struggling to survive.
Since COVID-19 in the United States emerged in the first months of 2020, social distancing and stay-at-home orders moved telehealth from a convenient option to an essential tool. Not only did telehealth allow many clinics to stay in business, it also assumed the critical role of creating access for patients who could not come in for therapy.
Some healthcare practitioners responded quickly to the opportunity. State and federal policies were adopted to make practicing and billing for telehealth easier. Insurance companies made changes too. Telehealth began gaining popularity, and many clinicians and patients embraced this new norm.
But we are not there yet. Even with its many benefits, some patients and clinicians have not accepted telehealth completely. It’s important to recognize the current reality, which is that telehealth has been introduced to mainstream America, and it is here to stay. As a clinician, you can either embrace the opportunity or be left behind to play catch up.
With measures in place to prevent infection and support social-distancing guidelines, some patients are becoming more comfortable with in-person visits. Even so, those clinicians who chose to adopt telehealth early have the ability to deliver a broader range of patient care and services in their clinics. If you haven’t moved to telehealth yet, it’s not too late. Here are some reasons why embracing telehealth is a good step to take today.
Benefits of Telehealth
Telehealth gives clinicians tools to engage patients remotely and improve patient experience and satisfaction. It also gives patients tools to connect with clinicians when time and convenience matter, when they want increased engagement, or when they have access challenges. Telehealth can be used as a stand-alone service or can be combined with in-person visits to diversify a patient’s care options.
Telehealth provides well-documented benefits for the patient:1, 2, 3, 4, 5, 6
- Improved access to care
- Reduced travel time
- Convenience
- Improved patient engagement
- Cost effectiveness
- Improved session attendance
- Care adaptable to the patient’s environment
In addition to these benefits, research conducted during the current public health crisis indicated that patients are highly satisfied with telehealth. In one study, one hundred patients completed a 21-question survey after a video‐based telehealth visit with a surgeon.7 The average score across all questions was 6.01 on a scale from 1 to 7, where 7 indicated the highest level of patient agreement. The highest scores were for questions related to patient satisfaction with telehealth (6.29).
[youtube v=”xUj-b7BneWQ”]
Patient Screening
Telehealth can be used as a screening resource to determine whether patients are appropriate to begin care or they need to be referred to a specialist. If they are appropriate for care, they can be scheduled for an in-person or a remote visit. If they are not yet ready for your clinical care, they can be referred to a specialist and return to you after their condition has been deemed appropriate for your services.
Watch the video below to learn more about how telehealth can be used as a screening tool to refer patients to a specialist.
[youtube v=”A3uJ_3IqP-8″]
Evaluation
Telehealth can be used for an evaluation of a patient who would prefer to be seen remotely instead of in-person. Whether the patient’s reason is accessibility (as is often the case with rural patients), a time constraint, or a disability, some circumstances make in-person visits more challenging.
COVID-19 has significantly impacted evaluations, as some patients are not comfortable leaving their homes or are hesitant to trust that a clinic will be able to maintain social distancing and safe contact. Again, telehealth provides a workable alternative.
Telehealth evaluations are similar to in-person evaluations where clinical reasoning is based on both the subjective and objective exams. Where they differ is that although a clinician can perform objective testing remotely, manual objective tests need to be modified during a telehealth visit. For example, palpating an area can be done by the patient while being guided and observed by the clinician.
Because some objective tests need to be modified in the telehealth environment, the subjective exam may influence clinical reasoning more than the objective exam measures. Based on the telehealth evaluation, the clinician will determine if the patient is appropriate for remote therapy or if they need a combination of remote and in-person care.
Watch the video below to learn more about the differences between in-person and telehealth evaluations.
[youtube v=”fIRl0T8XW1M”]
Follow-Up Sessions
Telehealth can be used in combination with in-person therapy during follow-up sessions to maximize session attendance and punctuality. It can be used with patients who have busy schedules, increased travel time, or just want to minimize social contact. This can impact recovery as well, since patients may get better quicker by increasing their quantity of visits and improving their compliance.
Watch the video below to learn more about how telehealth can be used as a tool for patient follow-up sessions.
[youtube v=”m8mbbl0nw0w”]
Discharge Planning
Telehealth can be used as a tool for patient monitoring as patients near discharge from therapy. Oftentimes, patients are discharged before their symptoms are fully resolved. Some patients reach a plateau during their care, begin missing appointments, and then abruptly disappear from the schedule. This patient attrition can be avoided by introducing patient-monitoring options toward the end of care.
Monitoring technology, such as wearable devices, can allow you to track a patient’s health metrics. These devices can be used to monitor heart rate, blood pressure, and other vitals as the deconditioned patient returns to normal activity. They can also be used to monitor step counts for patients who are returning to fitness programs after injury. Some devices can monitor distance run, stride length, cadence, and length and quality of sleep for athletes resuming training after an injury. These devices can even be used to monitor home-exercise compliance as some telehealth home-exercise platforms already integrate patient monitoring metrics. The data collected from a patient can be reviewed by a clinician during remote sessions, and based on patient responses, the clinician can indicate adjustments needed to therapy to optimize care.
Watch the video below to learn more about how telehealth can be used as a tool for patient monitoring as patients near discharge from therapy.
[youtube v=”I30DTrY6gR4″]
Telehealth Now
Telehealth is here to stay. For those who have not yet considered telehealth, the timing is perfect to embrace this new technology and add the viable, successful options it offers—for both patients and clinicians—to your clinic and practice.
Remember, telehealth can blend well with in-person visits anywhere in the clinical continuum. It can improve access to care and reduce travel time. It is convenient and cost effective. It improves session attendance and patient follow-up care. It is adaptable to the patient’s environment. And for you, the clinician, it positions you and your clinic in the future that is now.
Identify which of your patients are a good fit for telehealth. Decide where in the continuum telehealth best fits in your practice. Determine how you can add value for your patients by blending in-person care with telehealth.
The future of clinical care is here. Embrace the change.
Author
About Jared Vagy, PT, DPT, OCS, CSCS

Dr. Vagy received his Doctorate in Physical Therapy (DPT) from the University of Southern California (USC). He has completed a one-year residency in orthopedics and a one-year fellowship in movement science. Dr. Vagy is a Clinical Assistant Professor of Physical Therapy in the DPT program at USC. He has published three books and numerous articles on injury prevention. Dr. Vagy delivers lectures and seminars internationally on the topic of The Movement System. He is an orthopedic clinical specialist and a certified strength and conditioning specialist.
Dr. Vagy has served as a physical therapist in China for the Chinese National Track and Field Team, worked with USA Track and Field at the Olympic Team Trials, completed a rotation at the US Olympic Training Center working primarily with USA Men’s gymnastics, and provided medical care at international events such as the International Weightlifting Federation World Championships. He has rehabilitated several world champions, gold medalists, and Olympic athletes. His assessments and treatments are rooted deeply in an understanding of The Movement System.
References
- Bradford, N. K., Caffery, L. J., & Smith, A. C. (2016). Telehealth services in rural and remote Australia: a systematic review of models of care and factors influencing success and sustainability. Rural Remote Health, 16(4), 3808.
- Kairy, D., Lehoux, P., Vincent, C., & Visintin, M. (2009). A systematic review of clinical outcomes, clinical process, healthcare utilization and costs associated with telerehabilitation. Disability and Rehabilitation, 31(6), 427–47.
- Powell, R. E., Henstenberg, J. M., Cooper, G., Hollander, J. E., & Rising, K. L. (2017). Patient perceptions of telehealth primary care video visits. Annals of Family Medicine, 15(3), 225–229.
- Seto, E., Smith, D., Jacques, M., & Morita, P. P. (2019). Opportunities and challenges of telehealth in remote communities: case study of the Yukon telehealth system. JMIR Medical Informatics, 7(4), 311353.
- Morris, J., Grimmer-Somers, K., Kumar, S., Murphy, K., Gilmore, L., Ashman, B., & Perera, C., et al. (2011). Effectiveness of a physiotherapy-initiated telephone triage of orthopedic waitlist patients. Patient Related Outcome Measures, 2, 151–9.
- Guo, Y. & Albright, D. (2017). The effectiveness of telehealth on self-management for older adults with a chronic condition: A comprehensive narrative review of the literature. Journal of Telemedicine and Telecare, 24(6), 392–403.
- Layfield, E., Triantafillou, V., Prasad, A., Deng, J., Shanti, R., Newman, J. G., & Rajasekaran, K. (2020). Telemedicine for head and neck ambulatory visits during COVID-19: Evaluating usability and patient satisfaction. Head & Neck, 42(7), 1681–1689
- The original article and associated course can be found on the Medbridge blog page at this link: Click here





Leave A Comment